Glanzmann’s disease is a rare inherited bleeding disorder that affects the blood’s ability to clot properly. It occurs due to a deficiency or dysfunction of a specific protein on the surface of platelets, called glycoprotein IIb/IIIa, which is essential for platelets to clump together and stop bleeding. Because of this defect, individuals with Glanzmann’s disease experience abnormal bleeding even from minor injuries, and sometimes spontaneous bleeding can occur without any obvious cause.
This disorder is usually diagnosed in childhood, but the severity of symptoms can vary widely from person to person. Some individuals may have mild symptoms, while others may face life-threatening bleeding episodes. Because Glanzmann’s disease is genetic, it is passed down from parents to children, meaning there is currently no way to prevent its inheritance.
A very common question among patients and caregivers is whether Glanzmann’s disease can be cured. As of now, there is no complete cure for this condition, primarily because it is caused by a genetic mutation. However, medical advances have led to several treatment options that help manage bleeding and improve quality of life. Treatments such as platelet transfusions, medications to reduce bleeding, and in some cases, bone marrow transplantation offer hope for better control of the disease.
In this article, we will explore what Glanzmann’s disease is, its symptoms, how it is diagnosed, and the various treatments available today. We will also discuss ongoing research efforts aimed at finding more permanent solutions, including gene therapy. Finally, we will provide practical advice on living with this rare disorder and managing its challenges effectively.
What is Glanzmann’s Disease?
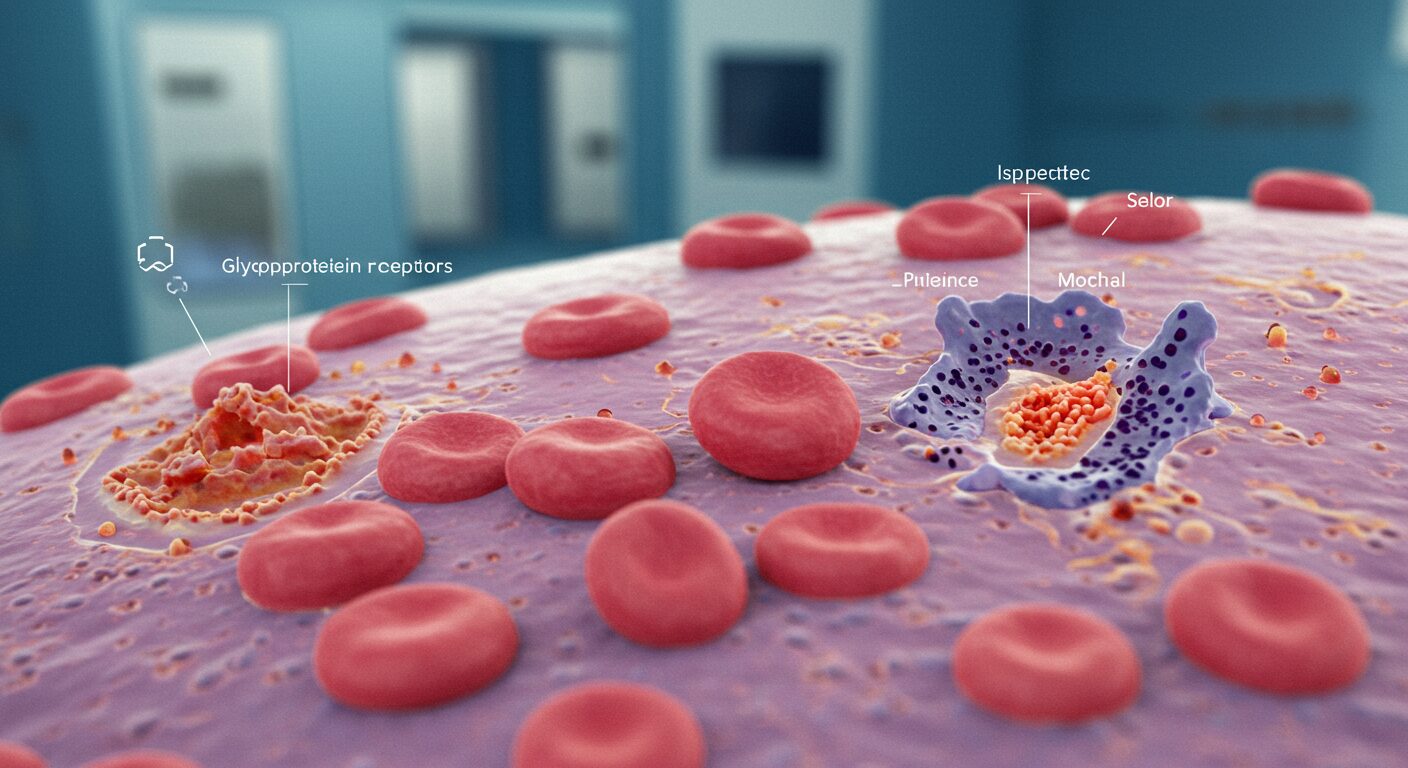
Glanzmann’s disease, also known as Glanzmann’s thrombasthenia, is a rare inherited bleeding disorder that affects the function of platelets in the blood. Platelets play a crucial role in stopping bleeding by clumping together at the site of a blood vessel injury to form a clot. In Glanzmann’s disease, this process is disrupted due to the absence or malfunction of a protein complex called glycoprotein IIb/IIIa on the platelet surface.
This protein complex acts like a bridge that allows platelets to stick to each other and form a stable clot. Without it, the platelets cannot clump properly, leading to defective clot formation and prolonged bleeding. Although the number of platelets in the blood remains normal in patients with Glanzmann’s disease, their ability to function is impaired.
Glanzmann’s disease is inherited in an autosomal recessive pattern. This means that a child needs to inherit two copies of the faulty gene—one from each parent—to develop the disease. Parents who carry one faulty gene typically do not show symptoms but can pass the gene to their children.
Because the disorder affects clot formation, people with Glanzmann’s disease can experience excessive bleeding after injuries, surgery, or dental work. In some cases, bleeding can occur spontaneously without any apparent trigger. The severity of the disease varies widely; some patients have only mild symptoms, while others face frequent and severe bleeding episodes.
Though Glanzmann’s disease is rare, understanding its nature is important for proper diagnosis and management. It is critical to differentiate it from other bleeding disorders like hemophilia or platelet function defects, as the treatment approach differs. Today, advanced blood tests, including platelet function assays and genetic testing, help confirm the diagnosis.
Symptoms of Glanzmann’s Disease
Glanzmann’s disease is primarily characterized by abnormal bleeding due to defective platelet function. Since platelets cannot clump together properly to form clots, even minor injuries can lead to excessive bleeding. The symptoms vary from person to person but generally include several common signs related to bleeding.
One of the most frequent symptoms is easy bruising. People with Glanzmann’s disease often develop large bruises even after minor bumps or without any obvious trauma. These bruises can be painful and take longer than usual to heal. Another common symptom is frequent nosebleeds (epistaxis), which may last longer or be more severe than normal. This can be particularly distressing, especially in children.
Bleeding from the gums is another common sign. Many patients experience bleeding during or after brushing their teeth or dental procedures. In females, heavy menstrual bleeding (menorrhagia) is a significant symptom that can affect quality of life and may lead to anemia if not managed properly.
In more severe cases, spontaneous bleeding can occur internally without any apparent cause. This may involve bleeding into the joints, muscles, or other organs, leading to pain and swelling. Internal bleeding episodes require immediate medical attention, as they can become life-threatening.
Some patients also experience prolonged bleeding after surgery, dental work, or trauma. The inability of platelets to form stable clots means that stopping bleeding during and after medical procedures can be very challenging.
It is important to recognize these symptoms early and seek medical advice. Because Glanzmann’s disease is rare and its symptoms overlap with other bleeding disorders, proper diagnosis is essential. Awareness of symptoms helps in timely diagnosis, which can lead to better management and reduced risk of complications.
How is Glanzmann’s Disease Diagnosed?
Diagnosing Glanzmann’s disease can be challenging because its symptoms often resemble those of other bleeding disorders. A detailed medical history and specialized blood tests are essential to confirm the diagnosis. Doctors start by asking about the patient’s bleeding history, including the frequency and severity of nosebleeds, bruising, bleeding after surgery or dental procedures, and family history of bleeding disorders.
Initial blood tests typically include a complete blood count (CBC) to check platelet numbers, which are usually normal in Glanzmann’s disease. However, normal platelet count alone does not rule out the disorder because the problem lies in platelet function, not quantity.
To assess platelet function, specific laboratory tests called platelet aggregation studies are performed. These tests measure how well platelets clump together when exposed to various substances. In Glanzmann’s disease, platelet aggregation is severely reduced or absent, confirming defective platelet function.
Flow cytometry is another important diagnostic tool. This test uses antibodies to detect the presence or absence of glycoprotein IIb/IIIa on the surface of platelets. A lack or severe reduction of this protein is a hallmark of Glanzmann’s disease.
In some cases, genetic testing may be done to identify mutations in the ITGA2B or ITGB3 genes responsible for producing the glycoprotein complex. Genetic tests can confirm the diagnosis and help with family counseling, especially in cases of consanguineous marriages where the risk of inheriting the disorder is higher.
Proper diagnosis is critical because treatment strategies differ for various bleeding disorders. Misdiagnosis can lead to ineffective treatments and increased risk of complications. Once diagnosed, patients can receive tailored treatment plans to manage bleeding episodes effectively and improve their quality of life.
Is There a Cure for Glanzmann’s Disease?
Currently, there is no universal cure for Glanzmann’s disease. Because it is a genetic disorder caused by mutations affecting platelet function, it cannot be completely reversed with medications or simple treatments. However, several options exist to manage symptoms and reduce bleeding episodes, improving the quality of life for affected individuals.
The most definitive treatment that can potentially cure Glanzmann’s disease is a bone marrow transplant (also called hematopoietic stem cell transplantation). This procedure replaces the patient’s defective blood-forming cells with healthy ones from a compatible donor. Since platelets are produced from bone marrow cells, this can restore normal platelet function and effectively cure the disease. However, bone marrow transplant carries significant risks, including graft-versus-host disease and transplant-related complications. It is usually reserved for severe cases where bleeding cannot be controlled by other means.
For most patients, management focuses on controlling bleeding episodes rather than curing the disease. Treatments include platelet transfusions, which temporarily provide functional platelets to help stop bleeding. However, repeated transfusions can lead to the body developing antibodies against donor platelets, making transfusions less effective over time.
Other treatment options include medications such as antifibrinolytic drugs, which help prevent the breakdown of blood clots, and recombinant activated factor VII (rFVIIa), which promotes clotting and can be used especially during bleeding episodes or surgeries.
Research is ongoing to develop gene therapies that may correct the genetic defect causing Glanzmann’s disease. While promising, these therapies are still experimental and not yet widely available.
In summary, while a complete cure is not currently accessible for most patients, bone marrow transplantation offers hope for some, and current treatments allow many individuals to live relatively normal lives by effectively managing symptoms.
Current Treatment Options
Managing Glanzmann’s disease requires a combination of treatments aimed at preventing and controlling bleeding episodes. Since a complete cure is rare, treatment focuses on improving quality of life and reducing complications. The main treatment methods include platelet transfusions, medications, and in some cases, bone marrow transplantation.
Here’s a suggested table based on the content:
| Treatment Option | Description | Benefits | Risks / Limitations |
|---|---|---|---|
| Platelet Transfusions | Transfused healthy platelets replace defective ones | Quick control of bleeding | Risk of alloimmunization, limited long-term use |
| Antifibrinolytic Drugs | Prevent breakdown of blood clots | Helps control mucosal bleeding | Mainly supports other treatments |
| Recombinant Factor VIIa (rFVIIa) | Stimulates clotting when transfusions fail | Effective for antibody-resistant patients | Expensive, needs careful supervision |
| Bone Marrow Transplant | Replaces defective marrow with healthy donor marrow | Potential cure | High risk, complex, possible rejection |
Platelet Transfusions
Platelet transfusions are the most common treatment used to stop or prevent bleeding in people with Glanzmann’s disease. Transfused platelets from healthy donors can temporarily replace the defective platelets and help form blood clots. This treatment is especially useful during surgery, after injuries, or during severe bleeding episodes. However, frequent transfusions can lead to the development of antibodies against donor platelets, a condition called alloimmunization, which makes future transfusions less effective and more complicated.
Antifibrinolytic Drugs
These drugs help reduce bleeding by preventing the breakdown of blood clots. Medications like tranexamic acid and aminocaproic acid are commonly used to support clot stability, especially for mucosal bleeding such as nosebleeds or gum bleeding. Antifibrinolytics are often given alongside other treatments to improve overall bleeding control.
Recombinant Activated Factor VII (rFVIIa)
rFVIIa is a clotting factor that can stimulate the clotting process in people with Glanzmann’s disease. It is particularly helpful for patients who have developed antibodies against transfused platelets and no longer respond well to transfusions. This medication is used during serious bleeding events or before surgeries to reduce bleeding risk. It has been shown to be effective in many cases but can be expensive and requires careful medical supervision.
Bone Marrow Transplant
For some patients with severe Glanzmann’s disease, bone marrow transplantation offers a potential cure. By replacing the patient’s defective blood-forming cells with healthy donor cells, normal platelet function can be restored. However, this procedure carries risks such as immune rejection and infection. It is generally considered only for patients with life-threatening bleeding who do not respond well to other treatments.
Challenges in Treating Glanzmann’s Disease
Treating Glanzmann’s disease comes with several significant challenges, mainly because of its genetic nature and the complexity of managing bleeding disorders. One of the biggest difficulties is that the disease affects platelet function rather than platelet count, making standard treatments less straightforward.
A major challenge is alloimmunization, which occurs when a patient’s immune system develops antibodies against transfused platelets. This immune reaction can make platelet transfusions ineffective or even dangerous, as the body rapidly destroys donor platelets. This complicates treatment, especially for patients who need repeated transfusions for frequent bleeding episodes or surgeries.
Another challenge is the rarity of the disease itself. Since Glanzmann’s disease is very uncommon, many doctors and healthcare providers have limited experience managing it. This can lead to delays in diagnosis, inappropriate treatment, or difficulties in accessing specialized care. Patients often need to be treated at specialized centers with expertise in bleeding disorders to receive the best care.
Additionally, some treatment options carry risks. Bone marrow transplantation, while potentially curative, involves serious complications including graft-versus-host disease, infections, and organ damage. The decision to undergo such a procedure requires careful weighing of benefits and risks.
Cost and availability of advanced treatments, such as recombinant factor VIIa and bone marrow transplants, can also limit access, particularly in low-resource settings. Moreover, the psychological and social impact of living with a chronic bleeding disorder adds to the patient’s overall burden.
Finally, ongoing research is needed to develop safer, more effective therapies, including gene therapy. Until such treatments become widely available, managing Glanzmann’s disease will continue to present significant challenges.
Research and Future Prospects
Research on Glanzmann’s disease is progressing steadily, offering hope for improved treatments and possibly a cure in the future. Scientists are exploring various advanced therapies, especially gene therapy, which aims to correct the underlying genetic defect causing the disease.
Gene therapy involves introducing a healthy copy of the faulty gene into the patient’s bone marrow cells. This technique could potentially restore normal platelet function by allowing the body to produce functional glycoprotein IIb/IIIa complexes. While still in experimental stages, early studies in animals and some clinical trials have shown promising results. If successful, gene therapy could provide a long-lasting or permanent cure without the risks associated with bone marrow transplants.
In addition to gene therapy, researchers are also investigating new medications that can better manage bleeding episodes with fewer side effects. For example, improved versions of recombinant factor VIIa and other clotting agents are under study to increase their effectiveness and reduce costs.
Another important area of research focuses on understanding how the immune system reacts to platelet transfusions. This knowledge may help develop treatments to prevent or reverse alloimmunization, making transfusions safer and more effective for patients who require them frequently.
Collaboration between researchers, clinicians, and patient organizations is crucial to advance knowledge and improve care for those with Glanzmann’s disease. Clinical trials continue to provide valuable data that can translate into better therapies and treatment guidelines.
Though a complete cure is not yet available for all patients, the future looks hopeful as science brings new possibilities closer to reality. Patients and families are encouraged to stay informed about ongoing research and consider participation in clinical trials when appropriate.
Living with Glanzmann’s Disease: Tips and Precautions
Living with Glanzmann’s disease requires careful management and lifestyle adjustments to minimize bleeding risks and maintain overall health. Since the disorder affects the body’s ability to form clots, even minor injuries can cause serious bleeding. Therefore, taking preventive measures is crucial.
First, people with Glanzmann’s disease should avoid activities with a high risk of injury or trauma. Contact sports, rough physical activities, or anything that may cause cuts or bruises should be limited or done with proper protective gear. Wearing helmets, pads, and other safety equipment can reduce the chance of injury.
Oral hygiene is another important aspect. Gentle brushing and regular dental checkups help prevent gum disease, which can lead to bleeding. Patients should inform their dentists about their condition before any dental procedures, so special precautions can be taken.
It is also essential to be cautious with medications. Drugs like aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) can interfere with platelet function and increase bleeding risk, so they should be avoided unless prescribed by a healthcare provider. Always consult a doctor before taking any new medication or supplements.
Maintaining regular communication with healthcare providers helps in managing the disease effectively. Patients should have an emergency plan in place for severe bleeding episodes, including access to treatments such as platelet transfusions or recombinant factor VIIa.
Additionally, emotional and psychological support is important. Chronic illnesses like Glanzmann’s disease can impact mental health, so seeking counseling or joining support groups can help patients and families cope better.
By following these tips and precautions, people with Glanzmann’s disease can lead safer and more comfortable lives while minimizing complications related to bleeding.
Conclusion
Glanzmann’s disease is a rare but serious bleeding disorder caused by defective platelet function. While there is currently no universal cure, advances in medical treatments have significantly improved the quality of life for many patients. Early diagnosis, careful management, and appropriate treatment options such as platelet transfusions, medications, and bone marrow transplants play a crucial role in controlling symptoms and preventing complications.
Challenges like alloimmunization, treatment risks, and limited awareness make managing the disease complex. However, ongoing research, especially in gene therapy and improved clotting agents, offers hope for more effective and potentially curative treatments in the future.
Living with Glanzmann’s disease requires caution, lifestyle adjustments, and support from healthcare providers and loved ones. With proper care and awareness, many individuals with this condition can lead fulfilling lives despite the bleeding risks.
Staying informed about new developments and maintaining regular medical follow-up can empower patients to manage Glanzmann’s disease proactively and safely.
FAQs About Glanzmann’s Disease
1. Is Glanzmann’s disease inherited?
Yes, Glanzmann’s disease is a genetic disorder inherited in an autosomal recessive pattern. This means a child must inherit the defective gene from both parents to develop the disease.
2. Can Glanzmann’s disease be cured?
Currently, there is no widespread cure. Bone marrow transplant may offer a cure for some severe cases, but most treatments focus on managing bleeding symptoms.
3. What are the common symptoms of Glanzmann’s disease?
Common symptoms include easy bruising, frequent nosebleeds, excessive bleeding from minor cuts, prolonged bleeding after surgery or dental work, and heavy menstrual bleeding in women.
4. How is Glanzmann’s disease diagnosed?
Diagnosis involves detailed medical history, blood tests including platelet function tests, flow cytometry to check for glycoprotein levels on platelets, and sometimes genetic testing.
5. What precautions should people with Glanzmann’s disease take?
Avoiding injury-prone activities, careful medication use, maintaining good dental hygiene, and having an emergency treatment plan are important precautions.







Leave a Reply